COVID-19: Lessons for the Global South
The larger trend shows that the Global South has yet to face the full impact of COVID-19. Are there any lessons to be learned from East Asia or the West, the earliest regions to become victims of the pandemic?
The Southern Hemisphere has suffered far too long from northern interference, first as commercial exploitation, then as colonialism, then as cultural arrogance, and now as expert knowledge purveyors. Therefore we should select lessons carefully on two criteria. First, the veracity and coherence of lessons, and second, the ability to apply them in other places, often far different in terms of incomes, political decision-making processes and infrastructures of transport and communication.
There are currently 1,898,029 coronavirus cases around the globe with 117,787 deaths associated with COVID-19. The majority of cases being in the United States, Spain, Italy, France and the UK. The Global North is experiencing the worst of the pandemic.
If we compare the two early and late coronavirus giants, China and the United States, the reported deaths in China are 18% to that of the U.S., despite the much longer period in which the virus has infected people in China. We define this as a measure of the vastly superior East Asian performance.
Given time and circumstance, such comparisons suffer from spurious accuracy but are no worse than claims to certainty based on even more dubious impressions. The advantages of the deaths to total cases ratio is that it is a rough but reasonable measure of the extent to which any nation or region has managed the virus effectively enough to reduce mortality over time, and to do so whilst increasing the accuracy of identifying total cases.
So, the death to total cases ratios are a proxy for the effectiveness of national medical and social policies and interventions that are not captured at all well in the mere numbers of cases.
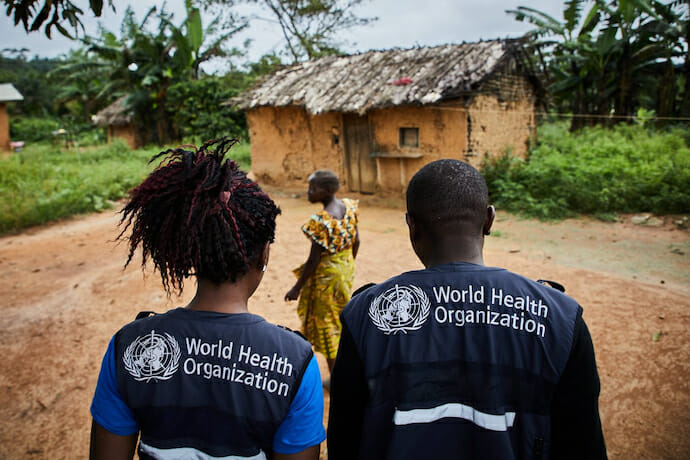
On such evidence to date, the Southern Hemisphere would do best to learn its lessons from East Asia rather than from the West. In East Asia what has stood out is the general effectiveness of early identification of the infected, tracing from external sources, and networking the identified contacts with other people, then using that for selected isolations, medicalisation (not necessarily hospitalisation) and more general social distancing.
This seems to have been very effective and far less costly than total lockdowns in the West. Despite being the first known epicentre, China is heavily populated, with natural commercial movement in the Hubei coastal province, as well as the special exigencies of the Chinese New Year. Even so, China now seems to be on the way to reopening Wuhan.
Secondly but related, social acquiescence was clearly higher in East Asia than in the West, giving much more potency to social distancing and voluntary isolation. This lowered all costs, with far less pressure on health services, which could focus more on very vulnerable older people and those who had underlying health issues.
Third, hospitalisation has been far less effective in the West by appalling absences of basic materials – protective clothing, masks and ventilators.
Fourth, East Asia’s emphasis on practicality and quick action even in situations of imperfect knowledge, seems to have been more appropriate than the Western dependency on scientific knowledge that often acted more to confuse than to guide interventions. The scientific forecasts of both government agencies and high-level research were often in seeming conflict and threaded in and out of stern warnings and rules-of-thumb that were coming from health systems and varied authorities. In East Asia, far more control was exerted by communities and civil society at large, less by policing and authority.
This should be observed and acted upon by Africa, South Asia, and South America. There is still time to intervene quickly and directly without recourse to ruinous expenditures. This is important. The average standard of living in seven Western nations with the highest COVID-19 infection rates is $50,719, measured in terms of purchasing power parity by the IMF. On the same measure, purchasing power in several East Asian nations averages $57,282.
In Africa, using the same measure, purchasing power lies at $5,467. Amongst the fourteen African nations with greatest virus cases, the average standard of living is $9,658 suggesting that those in Africa with higher incomes are no better off in terms of early COVID-19 invasion than are the very poor. This latter point might well arise from the higher incomes not compensating for the higher infection that arises from greater commerce and urbanism, as against the lesser infection in areas of lower-income but lower density and urbanism with better availability of very cheap local food supplies in small villages and townships.
Six large South American nations account for 56% of all the region’s cases and their proportion of deaths to total cases is low at around 4%. The standard of living in those nations is $17,959, just below the world average but they have suffered 45,158 coronavirus cases, which is three times the total number in Africa.
This confirms that relative national wealth and standards of living are not determining relative levels of infection or mortality. And it seems this is true amongst both rich and poor groups of nations. This, in turn, may suggest that expensive interventions are not the key and that social acceptance of official virus management procedures might be of much greater importance. This still leaves room for the importance of climatic and other natural variations amongst nations and regions.
The lessons to be learned can be summarised simply. Africa may have some advantages from large spaces and lower urbanism, but this is easily outweighed by a history of infectious diseases throughout Africa that is frankly appalling. More advantage lies with the local community and rural social systems that place great weight on respect for the sick and aged. This might well combine to reduce the registered ratio of deaths to total cases in many areas.
In poor urban areas the Western technique of lockdowns and closing of schools and businesses may be ineffective and – with greater surety – is the expensive option. East Asian experience points rather to social distancing and the need for very early direct intervention by local and central authorities. Effective identification and testing are more outcomes of careful organisation than of high incomes and expenditures. Africa can do this.